A year ago, the world was introduced to a new coronavirus causing an illness called COVID-19, generating untold illness and grief. The virus has exacted a devastating toll. The grim statistics from the beginning of the pandemic in America through 2/17/21 are:
- US deaths: 464,521
- US confirmed cases: 26,077,134
The 2021 average US life expectancy has decreased by one year when compared to 2019.
Tragically, this is only a part of the burden of the pandemic which has also caused emotional, economic, and educational disruption of an unprecedented degree in our modern society. Many of us have been changed and will most likely continue to feel these effects far into the future.
Thanks to a tremendous effort by scientists, healthcare providers, workers, leaders, and most of all the public, the rate of new cases and deaths has been on the decline. This is attributable to better public awareness, better treatments, better public health measures, and the arrival and utilization of new coronavirus vaccines.
Long COVID (Long-Haul COVID, Post-Acute COVID-19 Syndrome)
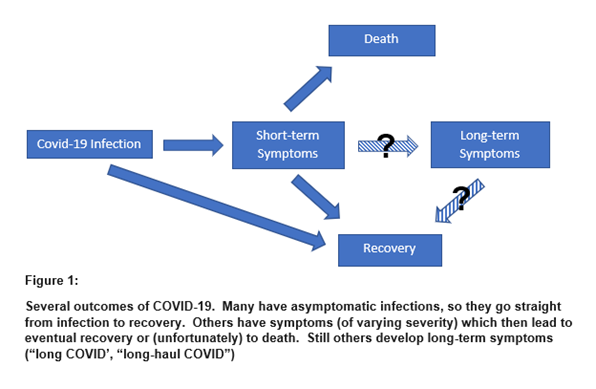
What is Long COVID? It is a constellation of various unique symptoms that persist weeks to months after infection with SARS-Cov-2 (the COVID-19 virus), not attributable to any other illness.
There are two types of long-COVID patients:
1) those who have permanently damaged organs due to viral infection and
2) those who have symptoms in the absence of obvious organ damage. In the case of people with recognized organ damage, it appears likely that a common mechanism involves inflammation of the blood vessels and blood clotting which is almost never seen in other respiratory viruses.
This article discusses long-COVID patients with ear, nose, and throat symptoms without obvious organ damage.
Additionally, at least one third of COVID-19 infections occur in patients that never developed symptoms, and this is known as the asymptomatic carrier state. Unfortunately, although an acute phase of this illness is not seen in these patients, they are nonetheless subject to possible development of long-COVID symptoms several weeks after their exposure and infection by the virus.
The CDC conducted a survey of symptomatic adults who tested positive for the coronavirus and who did not require hospitalization. After 3 weeks, 35% them had not returned to their baseline state of health following their initial infection. Of those people aged 18 to 34 years old, with no medical conditions, 20% had not returned to their usual state of health1. Overall, research has indicated that about a third of all people testing positive for the coronavirus have continued to have one or more symptoms—sometimes unrelated to their initial illness—three months after the acute phase of their infection has ended. The risk factors seem to be associated with developing long-COVID are: 1) initial presence of 5 or more symptoms of illness during the first week of infection, 2) increasing with age, 3) increasing with higher weight or obesity, and 4) female sex.
Ear, Nose, and Throat Doctors and Long-COVID
Ear, nose, and throat doctors are in a unique position to evaluate some of the early and late symptoms of the COVID-19 illness. Indeed, in many cases the initial symptom is loss of smell followed by decreased sense of taste.
In a recent study published in December, 20202 the prevalence of ear, nose, and throat symptoms in COVID-19 patients were noted. A subsequent study listed similarities in the symptoms of COVID-19 and other upper respiratory viral infections that involve the ear, nose, and throat.
The symptoms include fever (43% to 98%), cough (68% to 82%), fatigue (38% to 44%), sore throat (13.9% to 17.4%), dry cough (59.4%), sputum production (28% to 33%), loss of smell (51.2%), and loss of taste (47.1%). Generally, the recovery time for loss of sense of smell and taste was an average of 8 days.
Long COVID and loss of smell and taste.
According to an Italian study, about 10% of COVID-19 patients will have persistent smell and taste symptoms greater than one month after their initial infection. Although most patients recover spontaneously without the need for medical intervention, a significant number of patients have persistence of their symptoms and little is known about the prognosis and treatment of these symptoms. Like other respiratory viruses, loss of smell has been treated with topical nasal steroids.
Nomenclature:
Odorant: Something that smells.
Anosmia: Complete absence of the sense of smell.
Dysosmia: Parosmia (distorted smell of an odorant from the smell we expect) AND/OR Phantosmia (perceiving a smell that is not present).
In the case of COVID-19, in individuals that already have either chronic rhinosinusitis, recurrent acute sinusitis, allergic rhinitis, or nasal polyps, the use of a nasal steroid spray, nasal steroid irrigations, or oral steroid taper does seem to improve the sense of smell. However, in the case of long COVID anosmia patients without these pre-existing conditions, steroid treatment of the traditional type is not believed to be effective. This is because the loss of sense of smell is not related to nasal obstruction in COVID-19 patients.
A significant portion of COVID-19 patients will lose both smell and taste. This becomes a prominent symptom in some of the long-COVID population.
Whereas other viruses affect the smell sensory nerves (olfactory bulb neurons), COVID-19 results in damage to the supporting cells (sustentacular cells), surrounding the olfactory bulb neurons. This is good news since the sustentacular cells can be regenerated much more easily and rapidly than the olfactory bulb neurons:
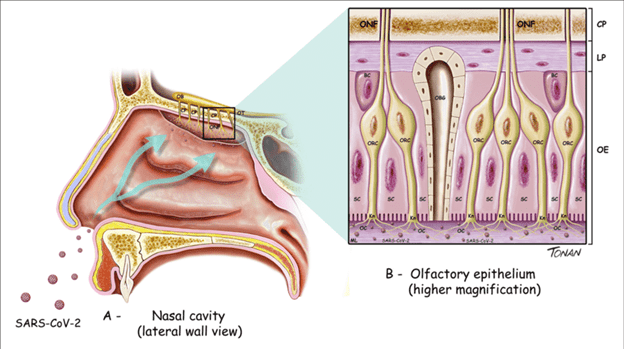
Figure 2:
Location of the smell sensory mechanism at the roof of the nasal cavity. The supporting cells (sustentacular cells) are colored purple and the olfactory neurons are colored brown.
Other approaches currently under investigation for mitigation of long-COVID anosmia include the use of zinc and vitamin B supplementation, vitamin A oils, steroid nasal rinses, and the use of compounded theophylline nasal spray.
The most promising approach to recovering smell in these patients is the use of olfactory training3. This is a technique that can be performed at home using a few simple substances (odorants) and it involves exposing the nose to the odor of these substances and imagining the previous sense of smell experience with these substances. The precise mechanism of this is not understood. Positive findings have been demonstrated in several well-controlled studies before and after the coronavirus pandemic. It is speculated that repeated stimulation of the olfactory neurons by clearly defined odors and may somehow improve regeneration or the ability of the brain to re-pattern previously lost pathways (a process called neuroplasticity).
Several websites exist to guide patients in olfactory training. Lemon, rose, clove and eucalyptus are the usual odorants provided in many cases as essential oils. British websites such as Abscent.org and fifthsense.org.uk provide training kits and information on performing the olfactory training, but such training can be learned and applied at home without a formal smell identification kit. Online dysosmia support groups may be found at: facebook.com/groups/AbScentCovid19 and facebook.com/groups/AbScentparosmia.
Interestingly, those patients who have dysosmia and older patients are believed to have an excellent prognosis4. Overall, the prognosis for recovery of functional sense of smell exceeds 90%.
Long COVID and Hearing Loss/Tinnitus
Ten percent of all COVID-19 adults report a change in their hearing status, at 8 weeks after diagnosis or hospitalization. Even some patients who have been completely asymptomatic have shown objectively measured decreases in their hearing.6 Strangely, patients who had asymptomatic COVID-19 infections had a greater likelihood of developing measurable hearing loss as time progressed after the initial infection. New onset tinnitus was noted and reviewed in 4 separate studies. Vertigo was noted in two studies. Many other studies have listed dizziness as a symptom, although it was unclear whether this was due to vertigo, imbalance, cardiovascular effects on blood pressure and heart rate, or neurological effects.
It is well recognized that many viruses such as measles, mumps, and rubella can cause hearing loss. Coronaviruses and herpesviruses can cause peripheral neuropathy and central nervous system effects. Conceivably COVID-19 could cause damage to the auditory nerve or central nervous system areas that are involved in processing of auditory signals and speech.
Long COVID and Shortness of Breath
Some long-COVID patients have persistent shortness of breath that lasts long after the acute phase of their disease has resolved. This is occurring in the absence of any significant findings on chest x-ray or chest CT scan and these patients were left without a therapeutic recourse. As proposed in a recent communication from two members of our ENT and Allergy Associates, LLP group--Dr. Jonathan Aviv and Dr. Sujana Chandrasekhar—the long-COVID symptoms of cough and shortness of breath may in part be mediated by damage to the vagal nerve-specifically the portion of the nerve that affects respiratory control and breathing at the entrance to the windpipe (trachea). The patients did not have shortness of breath at night and tended to experience shortness of breath after the inciting activity (talking, exercise, etc.). Drs. Aviv and Chandrasekhar proposed use of respiratory retraining as a useful adjunct to diminish the specific symptoms7.
The Future? Vagal Nerve Stimulation and COVID-19
The discovery 14 years ago of an “inflammatory reflex" involving central nervous system controls over the immune response stimulated research in ways that this neural network could be used to modulate or decrease inflammation. Cytokines are a broad and loosely defined organization of protein-like signaling molecules that control many aspects of inflammation. The reflex is an arc that is initiated by the presence of inflammation (cytokines) and this signal is transmitted to the central nervous system, which responds in a return arc to various immune organs (spleen, thymus, gut, etc.). There is also a release of a chemical—acetylcholine—which blocks certain initiation receptors on cells that make cytokines, resulting in a decrease in cytokine production. This information is carried by the vagus nerves (Latin: “the wanderer”).

Proof of Concept Posted on October 30, 2017, updated on Dec 7, 2017 by electrocore_admin
Figure 3: Location of vagus nerves in the neck, traveling from skull base through neck, thorax, and abdomen
The vagus nerve signal acts to suppresses the level of cytokines, therefore decreasing inflammation. An excess of cytokines (“cytokine storm’) is believed to responsible for much of the organ damage and long-term inflammation effects of COVID-19.
The vagus nerve can be electrically stimulated via electrodes placed on the outer ear via one of its branches, the greater auricular nerve.

Effect of Short-Term Transcutaneous Vagus Nerve Stimulation (tVNS) on Brain Processing of Food Cues: An Electrophysiological Study Martina A. Obst Front. Hum. Neurosci., 2020
Figure 4: Vagal electrodes in position on the external ear during vagal nerve stimulation.
This painless technique is called transcutaneous vagal stimulation. By supplying a repetitive low voltage, low amperage electrical stimulus to the ear over a period of 15 to 30 minutes a day, the vagus nerve can be modulated and is thought to have certain beneficial effects on inflammation, respiration, hypertension, cardiac status, anxiety, depression, epilepsy, pain, headache (migraine and cluster), and tinnitus (ringing or unwanted sound in the ears) among other disease processes.
An investigator has recently applied to the FDA for emergency use authorization for a trans-auricular vagal nerve stimulator attempting to modulate vagal nerve control of immune responses and cytokine storm8:

Nemechek P (2020) Vagus Nerve Stimulation is an Ideal Therapeutic Candidate for COVID-19 Infection. J Emerg Dis Virol 5(2): dx.doi.org/10.16966/2473-1846.152
Figure 5: Proposed injury pathways leading to organ damage after COVID-19 infection as mediated by excessive productions of chemical messengers called cytokines. The vagus nerves in part control overall regulation of cytokine production.
Another company has achieved FDA Emergency Use Authorization (EUA) for their transcutaneous vagal nerve stimulator. It is conceivable that this non-invasive, possibly effective, inexpensive, and simple treatment may be utilized to treat both acute COVID-19 infections and—eventually—long-COVID symptoms.
Summary
As specialists, ENT and Allergy Associates are in a unique position to assist patients with many long-COVID symptoms. We are the regional experts of the ear, nose. and throat and the experts on modulation of the immune system. Clearly, much remains to be understood about many aspects of this disease. However, there is a veritable torrent of research data such that one researcher described trying to integrate this data as like "drinking water from a fire hose". Today intensive research is ongoing in the hope that we can develop ever better therapies for our patients.
Bibliography:
1) Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network — United States, March–June 2020, Tenforde,M et.al., CDC COVID-19 Response Team, MMWR, July 31, 2020, Vol. 69, No. 30
2) American Journal of Otolaryngology, volume 41, issue 6, Erdal, S. et al. 2020,
3) Treatment of post‐viral olfactory dysfunction: an evidence‐based review with recommendations, Hura, N et al. Allergy and Rhinology 10, 1031-1120, September 2020
4) Parosmia is Associated with Relevant Olfactory Recovery After Olfactory Training, Liu, DT, Laryngoscope, 2020.
5) Systematic Review and Meta-analysis of Smell and Taste Disorders in COVID-19’ Ibekwe, TS, Oto-Open, Otolaryngology Head and Neck Surgery volume 4, number 3, September, 2020.
6) Does coronavirus affect the audio-vestibular system? A rapid systematic review Almufarrij,I, Kevin J. Munro International Journal of Audiology Volume 59, Issue 7, 2020
7) Covid-19 Era Post Viral Vagal Neuropathy Presenting as Persistent Shortness of Breath with Normal Pulmonary Imaging, Jonathan E Aviv, Sujana Chandrasekhar, and Byron Thomashow, International Journal of Pulmonary and Respiratory Sciences, volume 4, issue 4, October 2020.
8) Vagus Nerve Stimulation is an Ideal Therapeutic Candidate for COVID-19 Infection. Nemechek P, J Emerg Dis Virol 5(2), 2020: dx.doi.org/10.16966/2473-1846.152
Find an ENT & Allergy Associates Doctor Near You, or Explore More Blog Topics
