Parathyroid surgery is performed most commonly to treat primary hyperparathyroidism, a disorder where one or more the parathyroid glands becomes overgrown or overactive. Approximately 80% of patients with primary hyperparathyroidism have one of the four glands causing their problem. This means that in 15-20% of patients there may be 2 or more abnormal glands that need to be removed. Parathyroidectomy is performed though a horizontal incision in the lower part of the front of the neck, in an operating room in a patient under anesthesia. The surgery time may range from 1 to 5 hours, depending on how many glands need to be removed. In most cases a patient can be sent home the day of surgery. The goal of the surgery is to remove all of the abnormal parathyroid tissue and return the parathyroid hormone (PTH) level to normal.
Not everyone with primary hyperparathyroidism needs to have surgery. Patients with obvious symptoms such as easy fractures or kidney stones should clearly have surgery. Patients who are under 50 years old should have surgery because it is felt that they body will be subject to the disorder for so long that inevitably they will develop problems. Patients with very high blood calcium (>1mg/dl above normal) or urine calcium (>400 mg in a 24-hour urine collection) should have surgery. Patients with osteoporosis, even without factures, should have surgery to prevent future weakening of the bones. And patients with the beginnings of kidney damage and dysfunction should have surgery to prevent further damage. In patients who are asymptomatic and do not meet any of these criteria, observation is a reasonable option. Yearly testing to monitor progression of the disorder is done to identify problems as they arise. An asymptomatic person may also choose to have surgery, in an effort to avoid the problems that may occur.
In appropriately chosen patients, once the diagnosis of primary hyperparathyroidism is confirmed by blood work, planning for surgery can begin. Identifying which of the four glands is the culprit is important in an effort to make the surgery easier, quicker, and safer. A number of imaging modalities are used to try to identify the abnormal gland or glands. The most common are ultrasound, Sestamibi scanning, and CT imaging. The three modalities have individual strengths and weaknesses, and none of them are 100% perfect. However pre-operative imaging is routine and usually helpful in guiding the surgery. Abnormal parathyroid glands are visibly larger than normal glands, and directly identifying this during surgery is crucial. We are also able to check the PTH level in the blood during surgery. A PTH level is checked immediately prior to entering the operating room. After removing the suspected abnormal gland, another PTH level is drawn. If the PTH level drops to normal, it is an indicator that the remaining glands are normal. If the PTH remains elevated after removal of the first suspicious gland, additional abnormal glands need to be looked for.
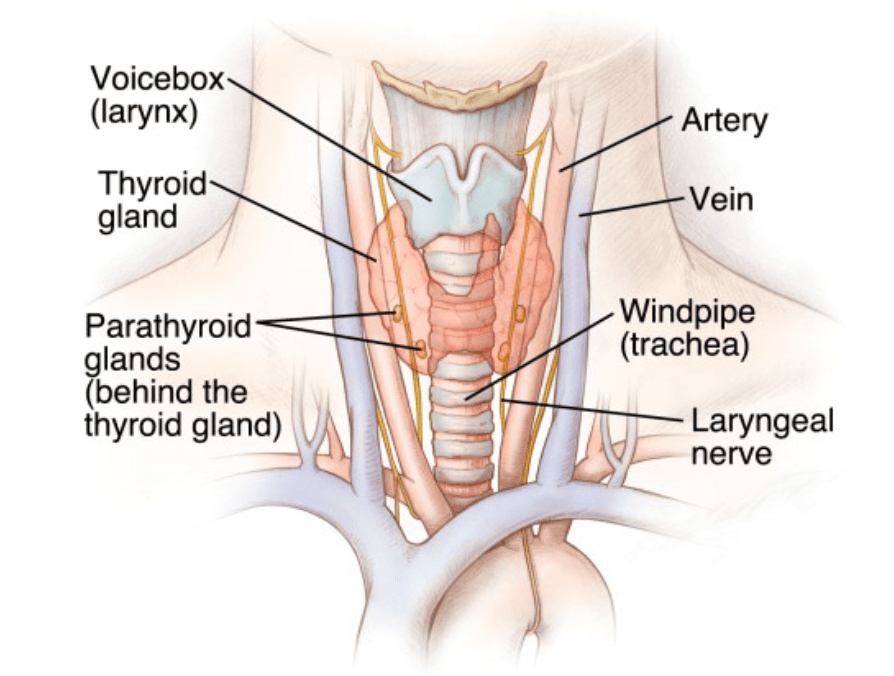
The success rate of parathyroidectomy is approximately 97%. Surgery can sometimes fail for a few reasons. In some cases, the abnormal parathyroid cannot be found. In the overwhelming majority of patients, the glands reside in a predictable location adjacent to the thyroid gland. However, there are case where, due to abnormalities of embryologic development, a gland can be located in an unusual place. Parathyroid glands can potentially be found anywhere from the jawline down to the area surrounding the heart. There are also times when a gland that looks, and is behaving, normally at the time of surgery becomes hyperactive in the months or years that follow. It is also possible, though very unlikely, that a person can have their parathyroid levels become too low after surgery. This can result in the need for long term calcium and vitamin D supplementation. There is a nerve, called the recurrent laryngeal nerve, that is located near the thyroid and parathyroid glands. This nerve controls the movement of the vocal cords. Injury to this nerve during thyroid or parathyroid surgery is possible, though extremely rare, occurring in significantly less than 1% of cases.
After parathyroidectomy patients should be less prone to kidney stones, and they should regain some of the bone density that has been lost. They may also feel less symptoms of fatigue, anxiety, and mental fogginess, though these symptoms are difficult to quantify. It is common for patients to have calcium levels that are slightly low after parathyroid surgery. The bones that have been depleted will begin to rebuild their calcium stores by pulling calcium out from the blood stream. We call this hungry bone syndrome. It is therefore routine to place patients on a low dose of calcium replacement after surgery. This may go on for months or years after surgery, depending on the extent of pre-operative bone density loss.
Most patients are sent home the day of surgery. If the operation requires removal of more than one gland, or lasts more than a few hours, it may be advisable to observe the patient overnight. Once a patient is discharged, there are very few restrictions. There will be a steri-strip (essentially a piece of white tape) over the incision. This is left in place and removed in the office the following week. Showering is allowed the day after surgery and it is OK for the site to get wet. Simply pat it dry after showering. A patient can eat and drink whatever they like and engage in whatever activities they feel up to. Typically, there is some moderate discomfort for the first few days, and pain medication is prescribed. Patients are usually back to work in one to two weeks.
Find an ENT & Allergy Associates Doctor Near You, or Explore More Blog Topics
